As appeared in the Winter 2022 issue of Scripts.
Introduction
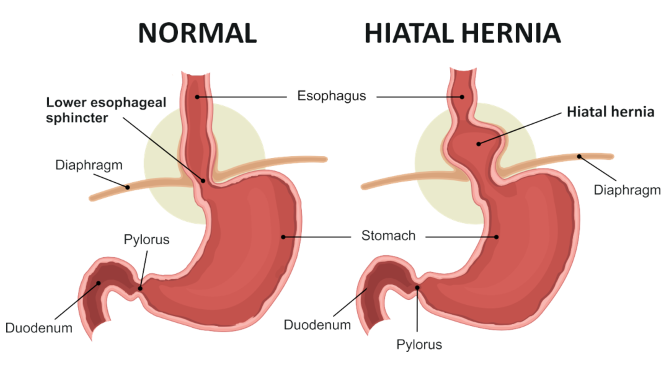
Hiatal hernias are hernias of intra abdominal contents through the diaphragm. The pathophysiology of development of a hiatal hernia can be somewhat complex. During swallowing the phrenoesophageal membrane is placed on tension and is stressed. The esophageal muscles shorten. All of which causes recoil of the gastroesophageal junction that pulls into the chest and then recoil to its normal position. The repetitive stress of swallowing, vomiting, straining can all lead to tearing or wear on the pherenoesophageal membrane leading its break-down and therefor a source of possible herniation.
Types of Hiatal Hernias
- Type I – Sliding hernia
This is defined by elevation of the gastroesophageal (GE) junction above the diaphragm. The remainder of the stomach remains in its typical position below the diaphragm - Type II, III and IV – Paraesophageal Hernias
- Type II – Defect in the phenoesophageal membrane (PEM) with herniation of the gastric fundus above the diaphragm with the GE junction in its normal position.
- Type III – Both the GE junction and the fundus of the stomach has herniated above the diaphragm
- Type IV – A large defect in the PEM with herniation of other organs besides the stomach into the chest such as colon, spleen, pancreas, small intestines, etc.
95% of Hiatal hernias are Type I and the remaining 5% encompass the type II-IV.
Symptoms
Heartburn, dysphagia of solids and at times liquids, regurgitation are most common with Type I hernias. Type II, III and IV can lead to epigastric or substernal chest pain, post prandial fullness, nausea, vomiting.
Complication
Bleeding, esophageal ulceration (Cameron Ulcers), metaplastic or dysplastic changes to the esophagus that could progress to esophageal cancer, volvulus, cardiac or pulmonary compression with resultant shortness of breath or changes in cardiac function.
Diagnosis
EGD, CT, Barium swallow all provide adequate imaging. The also will provide alternate diagnosis such as nutcracker esophagus, esophageal tumors, achalasia, peptic ulcer disease or gastritis.
Management
Asymptomatic hiatal hernias do not require repair. Surgical repair is indicated for symptomatic patients as listed above in which those symptoms are unable to be controlled medically. Indications for urgent repair are gastric volvulus, obstruction, bleeding, perforation or severe respiratory compromise.
Surgical Repair
Prior to repair, all patients require a proper work up. This includes EGD, Barium UGI, 24hr pH monitoring and esophageal manometry. These tests confirm symptomatic disease and rules out other esophageal disease that can be managed medically or a separate form of surgical correction.
Operative approaches include traditional open abdominal repair versus minimally invasive abdominal approach (laparoscopic or robotic). Some hernia repairs can also be approached from the chest. The decision making regarding the best approach has to do with surgeon preference and experience.
Minimally invasive repair accounts for greater than 90% of repairs done at this time. The length of stay, infection risk, re-operative risk, readmission, mortality are lessened by a minimally invasive repair. Trans-thoracic repairs have a longer hospital stay, higher postoperative need for mechanical ventilation and greater risk of pulmonary complications.
Repair types include repair of the hiatus primarily with or without mesh. 360 degree wrap of the stomach around the GE junction vs a partial wrap depending on the preoperative testing.
Outcomes
Minimally invasive repair mortality and morbidity rates are very low. 30 day mortality and morbidity for elective procedures are
0.8 and 1.7% respectively. Those numbers rise, not surprisingly for emergency procedures upwards to 5 and 28%. Transthoracic mortality and morbidity numbers are in the range of 2.1 and 1.7%.
Recurrence Rates
The rate of radiographic recurrence is much higher than that of clinically significant recurrence. Very few patients require repeat surgical intervention. Minimally invasive repair recurrence approaches 10% that is clinically significant and 25% radiographic recurrence. Open repair recurrence has been reported up to 44%. Transthoracic repair recurrence has been listed up to 2.1%.

