April is Testicular Cancer Awareness Month. Testicular germ cell tumors (GCTs) are the most common type of testicular cancers, affecting men ages 20-35. An estimated 9,760 new cases of testicular cancer will be diagnosed in the U.S. in 20241 and experts say incidence is rising, particularly among Hispanic men. However, because of the seminal discovery of combination chemotherapy by Dr Lawrence Einhorn in the 1970s, cure rates of advanced GCTs are over 80%, the highest in all solid tumors.2
Symptoms, diagnosis and staging
Men may present with testicular swelling, abdominal pain, back pain or respiratory symptoms depending on the extent of disease. Scrotal ultrasound, CT scans and serum tumor markers (STM) such as alpha-fetoprotein (AFP), human chorionic gonadotropin (HCG) and lactate dehydrogenase (LDH) are required for diagnosis and staging. Radical inguinal orchiectomy (surgery to remove a testicle) establishes diagnosis and serves as the initial therapy.
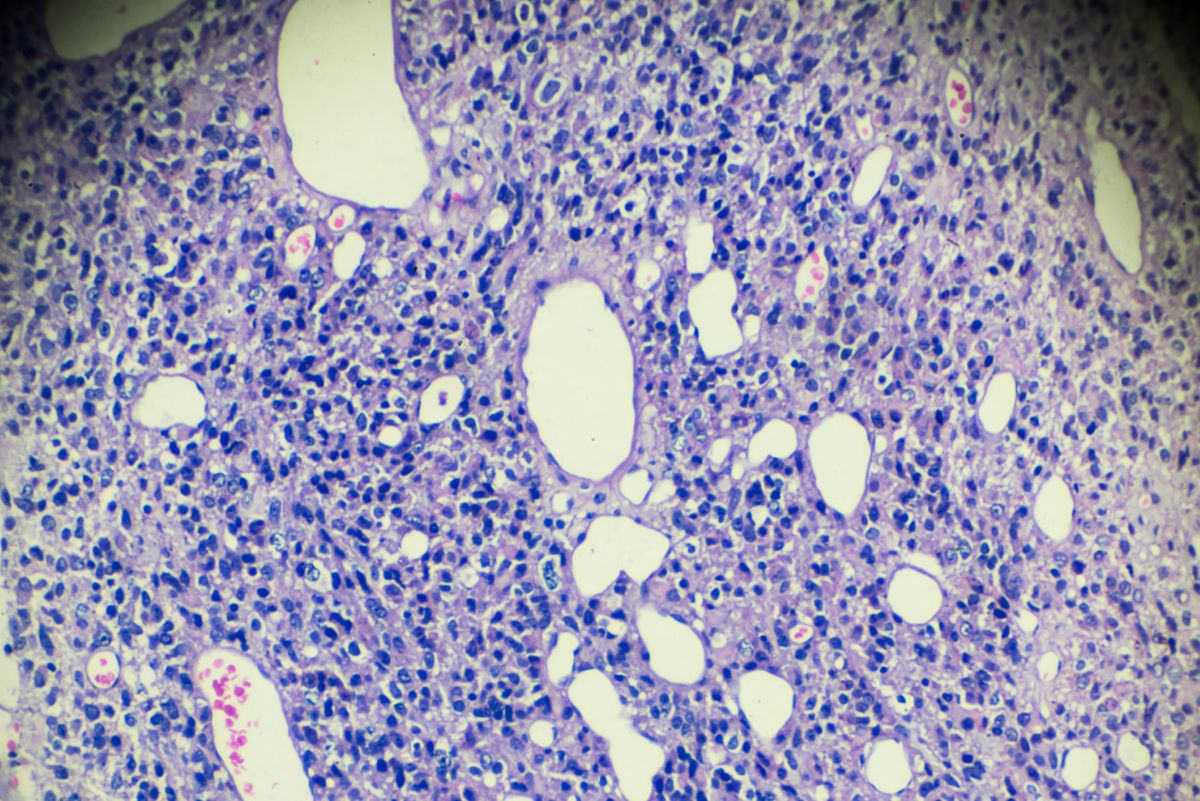
Histologically, GCTs are divided into seminomas or non-seminomas. The two types of cancer vastly differ in their therapeutic approach and prognosis. Features such as lymphovascular invasion, histologic subtype, tumor size and post-orchiectomy STM are used to predict metastatic recurrence of non-seminoma.
Testicular GCTs can spread to the retroperitoneal lymph nodes and lungs. Advanced disease is defined as the spread to extra-pulmonary organs such as the liver, bones and brain.
Treatment of early-stage GCTs
After orchiectomy, for men with stage 1 seminoma, active surveillance is preferred. Up to 15% of patients may progress on surveillance requiring further therapy. Adjuvant radiation or chemotherapy are established alternatives to surveillance but carry unnecessary long-term toxicities. Stage 1 non-seminoma is further divided into low-risk and high-risk groups. For low-risk stage 1A patients, surveillance is preferred. For high-risk patients defined by features such as lymphovascular invasion or embryonal carcinoma subtype, the risk of recurrence is higher up to 50%. Close surveillance versus chemotherapy regimen BEP for one cycle or retroperitoneal lymph node dissection (RPLND) are the three standard therapy options.
For stage 2 patients, systemic chemotherapy is offered especially if the tumor marker levels rise after orchiectomy. For stage 2 seminoma, recent studies support RPLND as an alternative to chemotherapy or radiation.
Surveillance of GCTs includes close monitoring of STMs and periodic imaging of the abdomen and chest. Recently a microRNA 371-3p was studied as a novel circulating tumor marker. It appears to be more sensitive than the conventional STMs but its validity as a marker for minimum residual disease after surgery is yet to be established.3
Treatment of advanced-stage GCTs
In contrast to other solid tumors, cisplatin-containing combination chemotherapy can be curative in a majority of men with metastatic disease. The established regimens include a combination of bleomycin, etoposide and platinum (BEP) or EP.
An international collaborative group IGCCCG stratified advanced GCTs into good, intermediate and poor risk groups based on pattern of spread, primary site and tumor marker levels. Men with good-risk disease require fewer cycles of chemotherapy as compared to those with intermediate or poor-risk disease. For men with non-seminoma, especially with presence of a teratoma component, post chemotherapy RPLND is required, if the imaging shows residual disease in the retroperitoneum.
Treatment of relapsed GCTs
Cure rates are as high as 50% with subsequent therapies in men who relapse after initial treatment. Conventional chemotherapy or high-dose chemotherapy followed by autologous stem cell transplantation are the two different treatment modalities. A prospective trial TIGER comparing the two approaches has recently completed accrual. The results are eagerly awaited.
Survivorship
Because GCTs are highly curable and affect mainly younger men, many patients face long-term survivorship issues. Infertility, hypogonadism, cardiovascular toxicities, psychological effects and long-term neurotoxicity of chemotherapy are the common long-term sequelae. These should be addressed even before the start of treatment. A strong survivorship program is an integral part of testicular cancer therapy.
Conclusion
Our understanding of genomic alterations, the discovery of new molecular targets, new disease monitoring tools such as circulating microRNA, and optimized sequencing of available therapies through ongoing prospective clinical trials is likely to help improve the treatment outcomes further.
Learn more about testicular cancer treatment at Northside Hospital Cancer Institute.
References:
- Siegel, Rebecca L., et al. "Cancer statistics, 2024." CA: A Cancer Journal for Clinicians (2024).
- Einhorn, L. H., et al. "Cis-diamminedichloroplatinum, vinblastine, and bleomycin combination chemotherapy in disseminated testicular cancer." Annals of Internal Medicine (1977).
- Dieckmann, K. P., et al. " Serum Levels of MicroRNA-371a-3p (M371 Test) as a New Biomarker of Testicular Germ Cell Tumors: Results of a Prospective Multicentric Study." Journal of Clinical Oncology (2019).