Receiving a diagnosis of a brain tumor can be overwhelming. In the U.S., approximately 700,000 people are living with a brain tumor, with around 87,000 new cases diagnosed each year. However, not all brain tumors are malignant. Meningiomas, for instance, are typically benign, meaning they are not cancerous. This guide provides an overview of meningiomas, their impact and available treatment options.
What is a meningioma?
Meningiomas are the most common primary brain tumors, accounting for 36-37% of all brain tumors. They originate from the meninges, the protective layers surrounding the brain and spinal cord. Although they can occur at any age, they are most frequently diagnosed in adults between 40 and 70 years old, with a peak incidence between 45 and 50. Women are more commonly affected than men, with a ratio of about 2 to 1.
Symptoms of meningiomas
Symptoms vary depending on the tumor’s size and location. Small or even medium-sized meningiomas might not cause noticeable symptoms and are often discovered incidentally during imaging for other conditions. When symptoms do occur, they may include:
- Headaches: Persistent headaches that do not respond to typical treatments.
- Seizures: Seizures may occur due to substantial brain irritation due to the presence of a tumor.
- Cognitive or personality changes: Tumors in the frontal lobe can lead to gradual changes in personality or cognitive function, often noticed by family members.
- Weakness or sensory changes: A meningioma pressing on brain areas responsible for movement or sensation may cause weakness, numbness or balance problems.
- Vision changes: Meningiomas near the optic nerves or those large enough to cause a substantial increase in intracranial pressure can result in vision problems.
- Cranial nerve dysfunction: Tumors at the skull's base can affect cranial nerves, leading to symptoms such as facial weakness, hearing loss or changes in facial sensation.
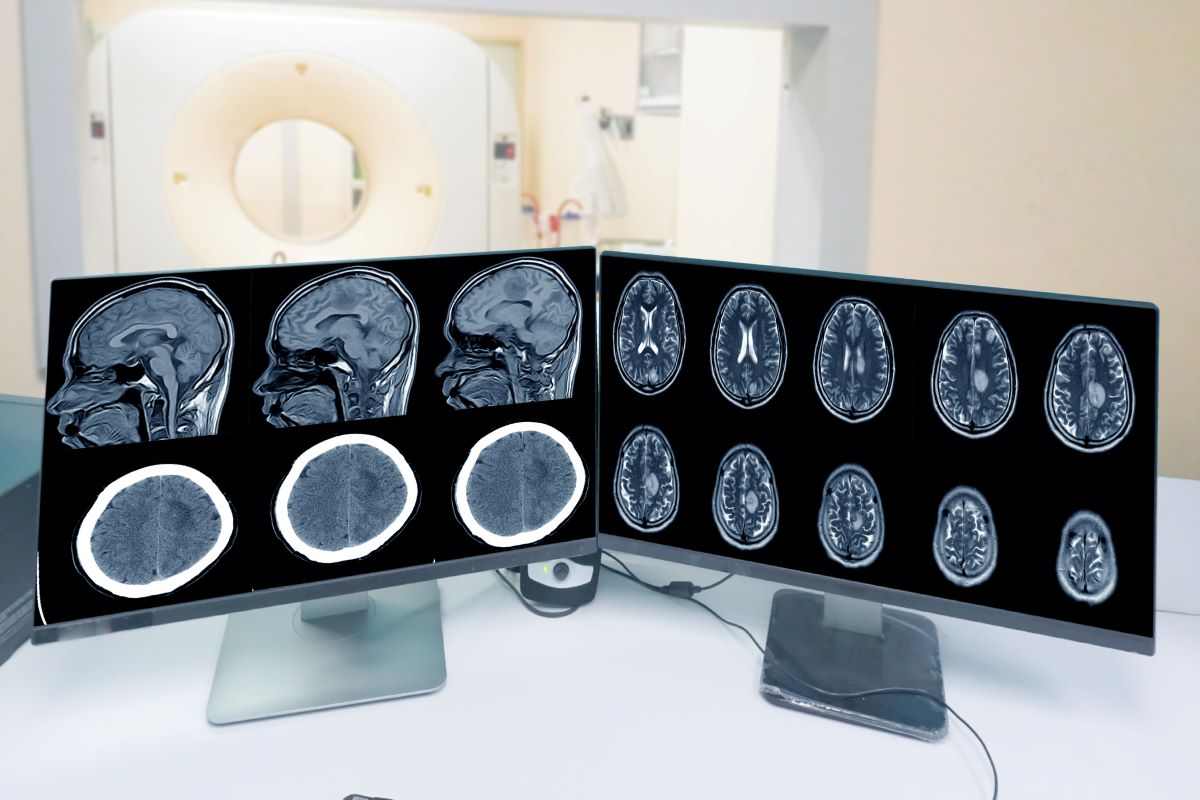
Diagnosis of meningiomas
A definitive diagnosis usually requires a biopsy. However, modern imaging techniques like MRI often suggest the presence of a meningioma with high accuracy. Meningiomas frequently show a characteristic "dural tail" on MRI, indicating attachment to the dura mater of the meninges.
Are meningiomas dangerous?
Most meningiomas are benign and grow very slowly, with an average growth rate of 1-2 millimeters per year. Approximately 80-81% are classified as Grade 1, meaning they do not spread to other parts of the brain or body and are the slowest growing. About 18% are Grade 2, often still benign but with a slightly higher chance of recurrence after treatment. Only around 2% are Grade 3, which are malignant and more aggressive.
What causes meningiomas?
The exact cause of meningiomas is not fully understood, but several factors may increase risk:
- Previous radiation exposure: Exposure to radiation to the head during childhood can elevate the risk of developing meningiomas later in life.
- Genetic conditions: Neurofibromatosis type 2 (NF2), a rare genetic disorder, can increase the likelihood of meningiomas.
- Hormonal factors: There is some evidence suggesting that hormones, particularly estrogen and progesterone, might influence meningioma growth. This might explain the observed loose association between meningiomas and conditions like breast cancer or the use of oral contraceptives or hormone replacement therapy, though the evidence is not strong enough to establish a definitive link.
Treatment options
Treatment for meningiomas depends on factors such as tumor size, location, growth rate and the patient’s overall health and age. Primary treatment options include:
- Observation (watchful waiting): For small, asymptomatic meningiomas, regular monitoring with MRI scans may be the best approach. Initially, an MRI is typically performed every few months after diagnosis, with annual scans if the tumor remains stable.
- Surgery: Surgery involves making an incision on the scalp and performing a craniotomy, where a portion of the skull is temporarily removed to access the tumor. Meningiomas in very specific locations may possibly accessed through the nose. Surgeons then use specialized tools and a microscope or endoscope to minimize damage to healthy brain tissue. Surgery is generally reserved for medium-to-large tumors causing significant pressure or symptoms. In some cases, smaller tumors may require surgery if their location could complicate future treatment or if symptoms necessitate immediate intervention. The goal is to remove as much of the tumor as possible, ideally achieving a gross total resection. If a Grade 1 meningioma is completely removed, it is often considered curative. Surgery also helps confirm the diagnosis and determine the exact grade of the tumor. However, surgery carries risks, particularly if the tumor is near critical structures like cranial nerves or major arteries and veins.
- Radiation therapy: Radiation therapy is an option for smaller tumors or those in difficult locations where surgery might be too risky. Modern techniques like stereotactic radiosurgery are highly precise, targeting only the tumor and minimizing damage to surrounding tissue. Radiation is also beneficial for patients who are not suitable candidates for surgery due to age or other health concerns. The primary goal of radiation is to halt tumor growth. Although it may not immediately shrink the tumor, it can prevent further enlargement over time.
Conclusion
Meningiomas are common, benign brain tumors that, while often slow-growing and non-cancerous, can still impact a person’s quality of life based on their size and location. Understanding your diagnosis and treatment options can help reduce anxiety and empower you to make informed decisions about your care. If you or a loved one has been diagnosed with a meningioma, working closely with your health care team is essential to determine the best course of action.
Learn more about brain tumor treatment at Northside.

