As appeared on MDAtl.com.
Weight loss surgery, or bariatric and metabolic surgery, continues to be refined as improved techniques and instrumentation evolve. Today, the surgeries are performed either laparoscopically or robotically, which allows for faster recovery times, fewer complications, shorter hospital stays and less pain.
Bariatric surgery is one of the most studied and scrutinized surgical disciplines due to many quality improvement initiatives from leading national societies, as well as the rapid increase in the number of cases being performed annually. Since 2011, there has been a continuous rise in the total number of weight-loss surgery operations being done in the U.S. In 2011, an estimated 158,000 cases were performed. That number has increased to 258,000 in 2019 and continues to increase as surgery has become more socially accepted, benefits are realized and the number of obese Americans continues to rise.
Surgical interventions can be seen as a spectrum in terms of amount of expected weight loss, complexity of the procedure and possible complications. There are a fair number of possible surgical options, but only a handful have been evaluated and studied enough to be recommended or endorsed by surgical societies. Those options include the adjustable gastric band, sleeve gastrectomy, gastric bypass, biliopancreatic diversion with duodenal switch, and single anastomosis duodeno-ileal bypass with sleeve gastrectomy.
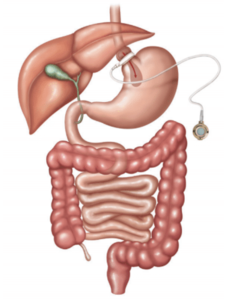 Adjustable Gastric Band
Adjustable Gastric Band
The adjustable gastric band (AGB) device is made of silicone and is wrapped around the upper portion of the stomach to limit the amount of food that can be eaten. The small gastric pouch above the band causes a feeling of fullness prior to the food entering the remainder of the stomach. It can be adjusted by filling the balloon around the stomach with saline to make it tighter and give more restriction.
Advantages of the lap band are that it has the lowest rate of early complications, is a same-day procedure, can be removed and has the fewest long-term nutritional concerns. The disadvantages are that the weight loss is much slower, it requires multiple adjustments, it is a foreign body that can move out of place or get dislodged, has a high rate of re-operation and can cause long-term swallowing issues and esophageal dilation.
The number of lap bands being placed has continued to decline over the last decade due to lower efficacy against comorbidities when compared to other options.
 Sleeve Gastrectomy
Sleeve Gastrectomy
Over the past 10-12 years, the sleeve gastrectomy has become the most widely performed bariatric procedure. It is performed by using surgical stapling devices to remove about 80% of the stomach, leaving the patient with a long, thin tube about the size and shape of a banana. This reduces the amount of food that can be consumed and also has a metabolic effect due to the removal of the portion of the stomach that produces ghrelin, the “hunger hormone.”
Advantages of the sleeve are that it is technically straightforward and reproducible, can be done on higher-risk patients, can be used as a bridge operation to gastric bypass or SADI-S and has a lower reoperation rate than other options. The drawbacks are that it is non-reversible, can increase issues with reflux and does not have as much metabolic effect as bypass operations.
 Roux-en-Y Gastric Bypass
Roux-en-Y Gastric Bypass
The Roux-en-Y gastric bypass (RYGB) has been used for more than 50 years. It is one of the most common procedures for weight loss and is one of the most studied and scrutinized operations performed.
To start, a small gastric pouch, about the size of an egg, is created from the very top of the stomach. A segment of small intestine is then reconnected to that gastric pouch. The bypassed part of the stomach and first part of the small intestine is then reconnected to the segment of small bowel about 150 cm away from the gastric pouch. This causes a restrictive weight loss, in that patients cannot eat as much, as well as a malabsorptive weight loss due to a shorter length of bowel having exposure to food and digestive enzymes to absorb nutrition and calories.
Benefits of the gastric bypass include better metabolic effects on diabetes and other obesity-related comorbidities, more sustained weight loss and a standardized operative approach.
Because it is a more complex procedure, there are more risks than the sleeve or lap band. There is a higher risk of nutritional and vitamin deficiencies, added risk of ulcers and small bowel obstructions, as well as the possibility of dumping syndrome if sugar and simple carbohydrates are consumed.
Biliopancreatic Diversion With Duodenal Switch
The biliopancreatic diversion with duodenal switch (BPD/DS) operation has historically been reserved for severe morbid obesity and for very hard-to-control diabetes. It is more complex and has more potential complications than the previously described procedures.
It is essentially a combination of sleeve gastrectomy and gastric bypass. A gastrectomy very similar to a sleeve is first performed. Then the duodenum is divided just past the pylorus. The small bowel is then reconnected in a way similar to the gastric bypass, but about 75% of the bowel is bypassed. This results in a significant decrease in absorption of calories and vitamins.
Advantages are that it has the strongest effect on gut hormones and diabetes, and has the most expected weight loss. But as a consequence to its effectiveness, patients are at much higher risk for vitamin and nutritional deficiencies requiring infusions, having significant loose stool and higher surgical complication risks, and reflux can become an issue.
Single Anastomosis Duodeno-ileal Bypass with Sleeve Gastrectomy
As the most recent bariatric operation to be endorsed by national surgical societies, single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) has the least experience and data behind it. It is very similar to BPD/DS but is a much simpler operation, as there is only one anastomosis.
A sleeve gastrectomy is performed first. Then the duodenum is divided just like in the BPD/DS. Then a loop of small bowel measured a few feet from the end is reconnected to the duodenum with one anastomosis.
This operation has similar advantages of BPD/DS, like good long-term weight loss and diabetic control, but is a safer operation and is a good option for revisions of sleeve gastrectomy. The disadvantages of SADI-S are that it is a newer operation with little long-term follow up, has increased issues with malabsorption and an increased risk of loose, frequent stool.